You’re showing up. You’re clean. You’re functioning.
But inside? You’re unraveling—quietly, invisibly.
For many high-functioning queer people, a Partial Hospitalization Program (PHP) feels like it should be enough. You’re doing the work, you’re saying the right things in group, and on paper, you’re stable. But if the care you’re getting isn’t speaking to your lived experience as an LGBTQ+ person—your queerness, your trauma, your mental health—then it might not be enough. Not because you’re failing, but because the program isn’t built to hold all of you.
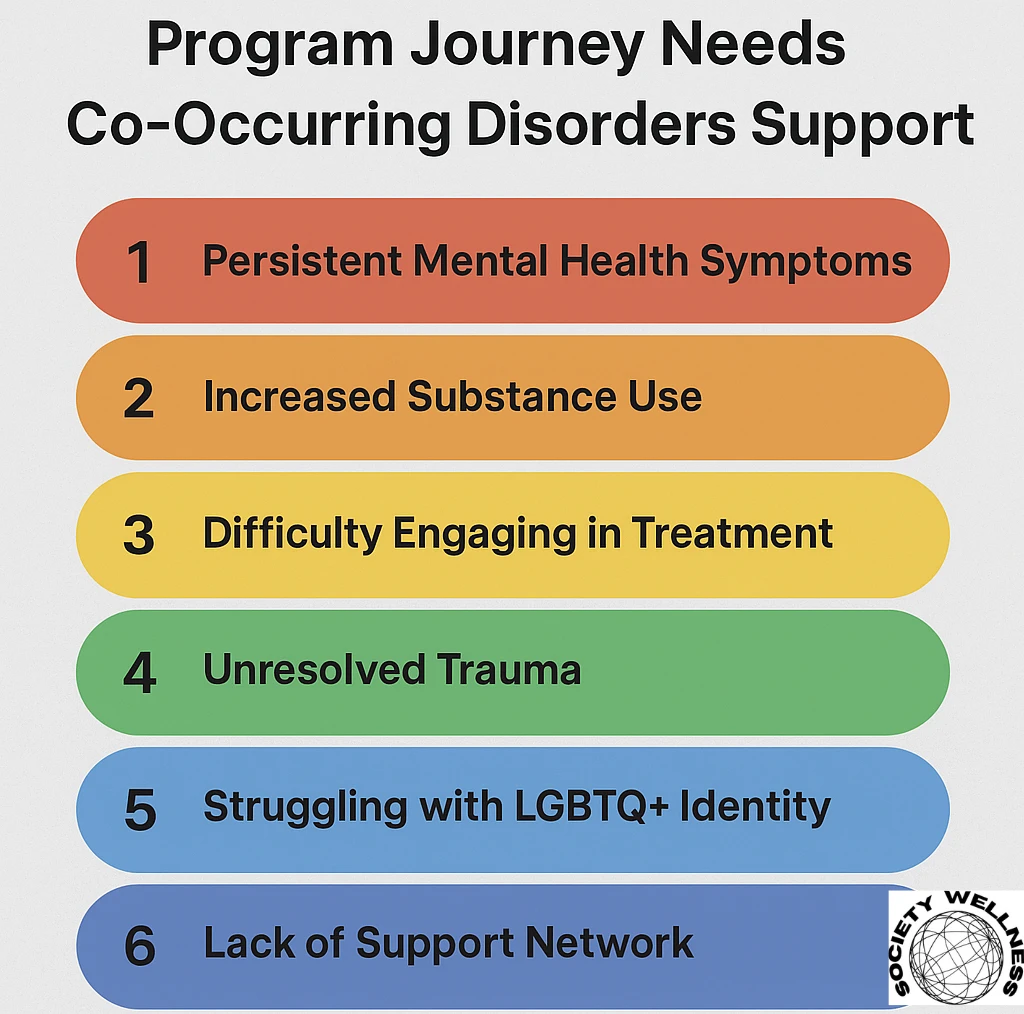
At Society Wellness Behavioral Health, our Partial Hospitalization Program in Needham is designed to treat co-occurring disorders through an LGBTQ+-affirming lens. Here’s how to know if it’s time to level up your support.
1. You’re White-Knuckling It Through the Day—And Calling It Progress
You’ve stopped using. You’re technically “doing well.” But inside, the anxiety is nonstop. The depression still knocks you out. You’re not living—you’re surviving. If you’re grinding your way through each day without relief, you might be facing untreated mental health conditions beneath the substance use.
And for many LGBTQ+ people, what looks like mental illness is often layered with the effects of chronic identity-based stress. Shame, internalized homophobia, gender dysphoria—these don’t show up neatly in an intake form. But they do affect your recovery.
2. You’re Filtering Everything in Group to Feel “Palatable”
If you’re constantly decoding the room—wondering, Can I say this? Will they get it?—you’re not in a space built for you. Maybe you soften your language around queer identity. Maybe you skip the part where the trauma started before the substance use, when your family rejected you. Maybe you joke instead of cry.
If you’re editing yourself in group to avoid awkward silence or blank stares, it’s not your fault. It’s the program. And you deserve one where you don’t have to translate your truth.
3. You’ve “Recovered” But Still Feel Disconnected From the LGBTQ+ You
Some of us used to drink to be social in queer spaces—or to survive them. For others, substances dulled the edge of gender dysphoria or masked the pain of erasure.
Now that you’re sober, you might be realizing: you don’t know how to connect to the LGBTQ+ community without using. Or you don’t feel like you belong in either world—queer spaces or sober ones. That disconnection isn’t failure. It’s a signal that identity-affirming, dual-diagnosis care could help bridge that gap.
4. You’re Still Carrying Old Shame—And It’s Getting Louder
Maybe no one in group is saying anything explicitly harmful. But no one’s talking about what it’s like to be queer and navigating sobriety either. That silence? It creates space for old narratives to creep back in:
- Maybe I’m too much.
- Maybe my pain isn’t valid.
- Maybe I should just be grateful I’m sober.
If your inner critic is still shouting—and you’re too afraid to say so out loud—your PHP might be missing trauma-informed, LGBTQ+-affirming therapy that lets you unpack why that voice is still running the show.
5. You’re “Stable” But Numb
Your days are structured. Your chart looks fine. But emotionally? You feel flat. Disconnected. Like you’re watching yourself go through the motions.
For many queer clients, this emotional blunting is the cost of being in spaces that never reflected them. You got good at surviving—at blending in. But healing requires connection, not just compliance. If you’re numb, it might be time for psychiatric evaluation, deeper therapy, or community-based programming that reconnects you to joy.
“I didn’t just need to stop drinking. I needed to figure out why being sober made me feel invisible.”
– PHP Client, 2024
6. Your LGBTQ+ Identity Isn’t Part of the Treatment Plan
This one’s subtle—but crucial.
If your treatment plan talks about trauma but not coming out…
If your therapist knows your triggers but not your pronouns…
If your group accepts you but never names queerness as a factor…
Then your care is incomplete.
Being LGBTQ+ isn’t a footnote. It’s part of your story. And effective dual-diagnosis care should treat it that way—not as a complication, but as a core part of your healing.
7. You’re Tired of Being the Educator
If you’re the one explaining terms, correcting assumptions, or bringing the queer lens into every conversation—you’re not in the right program. It’s not your job to educate your providers. It’s their job to create a space where you don’t have to.
You deserve care that already understands how being queer, trans, or gender nonconforming can shape your mental health and substance use patterns. Not care that sees you as “just another client.”
PHP Isn’t One-Size-Fits-All—Especially If You’re LGBTQ+
At Society Wellness Behavioral Health in Needham, Massachusetts, we built our Partial Hospitalization Program with LGBTQ+ clients in mind. That means queer-affirming therapists. Trauma-informed group spaces. And integrated support for co-occurring disorders that acknowledges your full, complex self.
Because real recovery isn’t just about getting sober—it’s about feeling seen.
📞 Ready to feel seen and supported?
Call (888) 964-8116 or visit our Partial Hospitalization Program page to learn more about LGBTQ+-affirming PHP services in Needham, Massachusetts.

