Collapsed veins are a significant medical issue often experienced by individuals who inject drugs. This condition occurs when the walls of a vein collapse or become damaged due to repeated trauma, preventing proper blood flow. This blog will provide a detailed understanding of what a collapsed vein is, the risks associated with it, and the potential signs and symptoms. Moreover, for the LGBTQ+ community, this issue can be compounded by societal stigmas and stressors that make access to safe medical care more difficult, further emphasizing the need for awareness and early intervention.
What Causes a Collapsed Vein?
A collapsed vein can happen for various reasons, particularly due to repeated intravenous drug use. Injecting drugs like heroin, methamphetamine, or even prescription medications using non-sterile techniques can result in severe damage to veins. Over time, constant pressure and trauma from needles can weaken and destroy the structural integrity of the vein.
Some common causes of collapsed veins include:
- Frequent Injection into the Same Vein: Overuse of a particular vein leads to scarring and weakening, making it more prone to collapse.
- Improper Needle Use: Using blunt or non-sterile needles can damage the vein and surrounding tissue, leading to infection or collapse.
- Large Volume Injections: Injecting too much fluid at once can put excessive pressure on the vein, causing it to collapse.
- Improper Injection Technique: Injecting drugs improperly or too quickly can lead to vein damage.
- Underlying Health Conditions: Health conditions such as diabetes or clotting disorders can make veins more susceptible to damage.
Short-Term and Long-Term Risks of Collapsed Veins
The short-term risks of collapsed veins can be immediate and painful, often leading to complications such as swelling, bruising, and difficulty finding other usable veins for future injections. But it doesn’t stop there; the long-term risks of collapsed veins are much more severe and can lead to chronic health issues.
Some of these include:
- Blood Clots and Deep Vein Thrombosis (DVT): Damaged veins are more susceptible to clot formation, which can lead to life-threatening conditions like DVT or pulmonary embolism if a clot travels to the lungs.
- Permanent Vein Damage: If veins collapse repeatedly, they may not recover, leading to permanent loss of function and forcing individuals to seek alternative, often more dangerous, injection sites such as neck veins.
- Infections and Abscesses: Collapsed veins can lead to bacterial infections or abscesses, especially if individuals continue to inject into damaged tissue, increasing the risk of life-threatening conditions like sepsis.
- Reduced Blood Flow: When a vein collapses, it can affect circulation in the surrounding area, potentially causing tissue death or necrosis if not addressed promptly.
- Loss of Limb Function: In severe cases, repeated injection into collapsed veins can result in reduced mobility and functionality in the affected limbs.
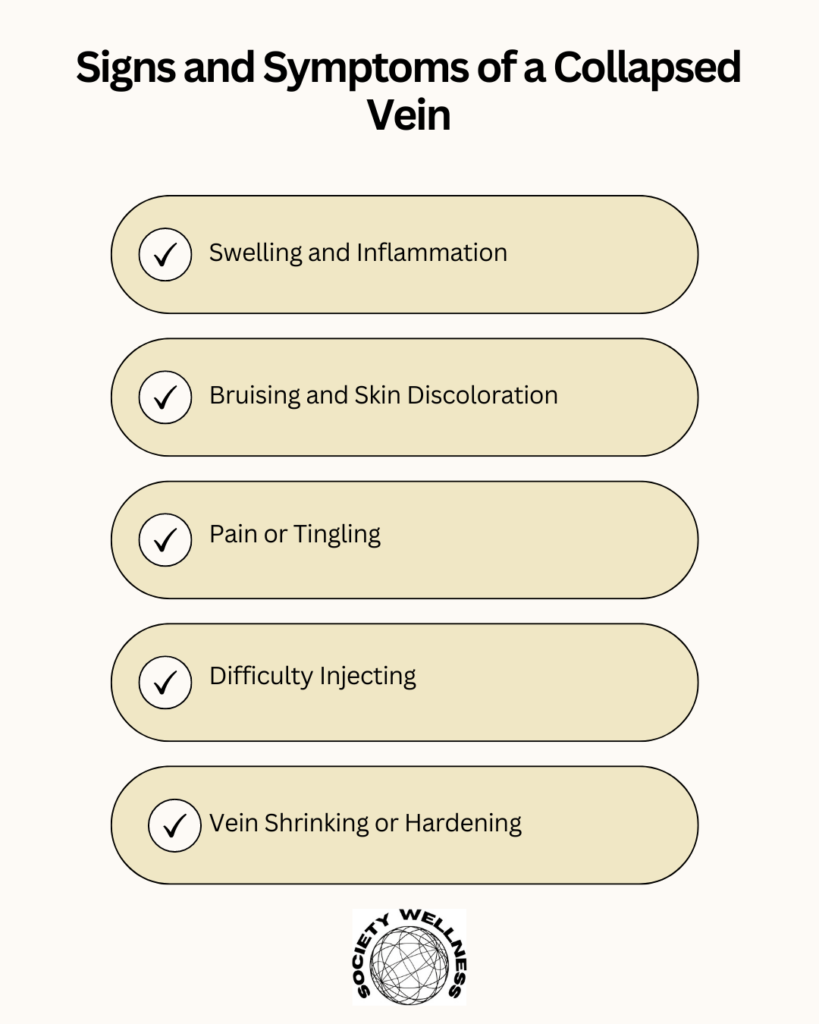
Signs and Symptoms of a Collapsed Vein
Recognizing the signs and symptoms of a collapsed vein is crucial to getting prompt medical help. Some symptoms may present immediately after an injection, while others may develop more slowly.
Here are the most common symptoms:
- Swelling and Inflammation: A collapsed vein prevents proper blood flow, causing swelling at the site of injection. The area may also feel warm or tender to the touch.
- Bruising and Skin Discoloration: Collapsed veins often lead to bruising and discoloration. These can appear as dark purple, blue, or even black marks around the injection site.
- Pain or Tingling: When veins collapse, the surrounding tissue often becomes painful, especially when pressure is applied. Individuals may also experience tingling or numbness in the area.
- Difficulty Injecting: Injecting into a collapsed vein becomes difficult, and the syringe may not draw back blood when attempting to inject, indicating the vein has lost functionality.
- Vein Shrinking or Hardening: Over time, the vein may become less visible or even harden due to scarring, making it more difficult to locate for future injections.
- Visible Scarring and Track Marks: Repeated injections into the same area often result in track marks or visible scarring, which may indicate that veins have collapsed.
Treatment Options for Collapsed Veins
Once a vein has collapsed, there is often no way to repair the damage, but there are treatment options to manage the symptoms and prevent further complications.
- Immediate Medical Intervention: In the event of a collapsed vein, it’s essential to seek medical attention, especially if there is pain, swelling, or signs of infection. A healthcare provider may prescribe antibiotics for infection or recommend rest and avoiding injection into the same area.
- Hot Compresses: Applying a warm compress can improve blood flow to the area and reduce swelling. This is especially helpful in the early stages of vein collapse.
- Avoiding Further Damage: The best way to treat a collapsed vein is to avoid further damage. Avoid injecting into the collapsed vein or switching to alternative methods like medication-assisted treatment (MAT) under medical supervision.
- Medical Evaluation for Clots: If there is a suspicion of a blood clot, a doctor may order tests like an ultrasound or CT scan to ensure no deep vein thrombosis or other clot-related issues.
- Substance Use Treatment and Harm Reduction Programs: Seeking professional help for drug addiction is critical in preventing the recurrence of collapsed veins. Many LGBTQ-friendly addiction centers offer harm-reduction services and addiction treatment programs that emphasize safe injection practices.
LGBTQ+ Addiction Treatment Programs for Intravenous Drug Use
At LGBTQ Addiction Centers, we offer a range of addiction treatment services specifically designed for the LGBTQ+ community. Our programs are not only focused on physical health but also address the unique mental health challenges LGBTQ+ individuals face during recovery.
- LGBTQ+ Substance Abuse Treatment Programs: We offer tailored treatment options for those struggling with substance use, particularly those injecting drugs, to minimize harm and support recovery.
- Day, Night, and Evening Treatment Programs: Our variety of treatment programs ensure that no matter your schedule, you have access to professional care that fits your lifestyle and recovery needs.
- Mental Health Programs: Many individuals who inject drugs also struggle with mental health issues such as anxiety, depression, or trauma. Our comprehensive LGBTQ+ Mental Health Programs include therapies like Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) to address these underlying mental health conditions.
- Medical Detox and Harm Reduction: Our detox programs provide a safe space to withdraw from drugs while receiving 24/7 medical supervision. We also offer harm-reduction education to minimize the risks associated with drug use, such as vein collapse.
Conclusion
Collapsed veins are a serious complication of intravenous drug use, and without intervention, they can lead to long-term health problems. If you or a loved one is struggling with substance abuse and experiencing complications like collapsed veins, seeking help is essential.
At LGBTQ Addiction Centers, we provide compassionate, inclusive care specifically designed for the LGBTQ+ community. Our team of medical professionals and therapists is here to support you with a range of treatment programs that address both the physical and emotional aspects of recovery.
Reach out or call us at:(888)964-8116 today to learn more about our LGBTQ Addiction Treatment Programs and start your journey toward a healthier, substance-free life.
FAQ on Collapsed Veins
What are collapsed veins?
Collapsed veins occur when the walls of a vein collapse or become damaged, preventing proper blood flow. This is often a result of repeated intravenous drug use or trauma.
What causes a collapsed vein?
Common causes include frequent injection into the same vein, improper needle use, large volume injections, and underlying health conditions such as diabetes.
What are the symptoms of a collapsed vein?
Symptoms can include swelling and inflammation, bruising or skin discoloration, pain or tingling, difficulty injecting, and visible scarring or track marks.
What are the risks associated with collapsed veins?
Risks include blood clots, permanent vein damage, infections, reduced blood flow, and loss of limb function.
How can collapsed veins be treated?
Treatment may involve immediate medical intervention, applying hot compresses, avoiding further damage, and seeking substance use treatment.
What should I do if I suspect I have a collapsed vein?
It’s essential to seek medical attention as soon as possible, especially if you experience pain, swelling, or signs of infection.

